I slept something like 9.5 hours last night.
It was really wonderful. And I woke up feeling better. It’s very odd, vacillating between sadness (mix of fear / loss / uncertainty / feelings of inadequacy, I think) and gratitude that right now — for the most part, within my family and loved ones — everything is so far okay.
Josh is off today and I am technically off (our health system is asking every provider to take 1 PTO day/pay period unless they are absolutely on the front lines — ID, ICU, ED, etc) so my 0.9FTE is now essentially 0.8. I have a couple of meetings but will try to lie low in the spirit of actually taking the time off.
A few of us ran a narrative medicine / wellness session with the residents yesterday. We asked them to share their fears. NO ONE bought up the one that haunts me frequently (feelings of inadequacy/incompetence in the face of desperate need on the front lines, or in more concrete terms, fear of being asked to work in the ICU). I couldn’t tell if that was because they were too embarrassed to admit something like that with their program director and other leadership listening, or because their generation isn’t as saddled with this thought pattern?
Is imposter syndrome a generational thing? (Not that I truly am qualified to be an ICU physician, but in reality I’m probably the same degree of unqualified as all of my pediatric sub-specialist peers). Gender is not the issue because 75% of the residents on the call were women.
Anyway, it was interesting. And I shared my own thoughts, hopeful that they would help someone, but now I’m also worried that they will think their PD is overly neurotic and/or anxious.
Oh well.
Today:
- Workout with Josh (took last 2 days off but it’s time to get back on the Beachbody horse)
- Help kids with school
- Work on resident schedules for next year
- Possibly attend one of my afternoon meetings today while walking around the neighborhood. I did this yesterday with a Zoom session and found I was able to concentrate as well or BETTER (because I was not tempted to check email / phone / etc while listening since I was walking!).
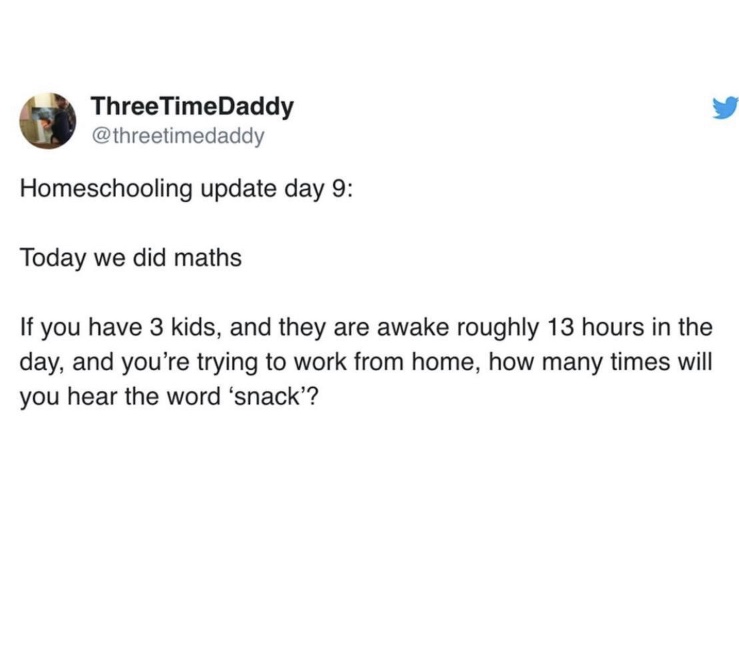
We will end today’s post with some humor:


(already planning some fancy takeout!)
PS: My call coverage week is over until next Tuesday when I have a week of my own call. Will be a mix of in-person and phone/video as much as I can do it.

15 Comments
I think your residents likely appreciated your honesty and candor. I think it’s hard to be vulnerable and share your fears when you are in a junior position… So I would not worry about them thinking you are neurotic! We had a big call yesterday with a senior leader with a Q&A session and there were very few questions. I think people are afraid to speak up at times, even though many of the people on the call were fairly seasoned/more senior people. In our case, our CEO had recently said that we will lose $1b in revenue so need to cut $700 million in costs so now people are pretty worried/paranoid about job cuts so I think they are especially unlikely to speak up… :/
I think you’ll need to just stay 39 this year and celebrate your 40th next year. 😉
That one about the baby boom being first born children made me laugh out loud! Being home with a toddler and Grade 1 makes me super comfortable with the choice of 2. YUP!!
And i am also 40 this year so the Friends style shirt is very apt (but i am in June but hardly expect things to be ‘normal’ by then. Mayyyybbbbeee transitioning … anyway, cheers to an at-home birthday
It was probably a mixture of feeling that they can’t be vulnerable in front of you and their peers for some, and a feeling of invincibility and that everyone else is weak and they are strong thinking among the others. I’ve been really surprised (and touched) the degree to which the residents I’ve been talking to have been willing to share their fears with me, but maybe it makes sense because a) I am closer to them in the hierarchy to them, b) I make myself available to them with my physical presence not just during official meetings, and c) these were interpersonal conversations between people moreso than between a program director and resident. The hierarchy really matters so much, and it is everywhere. I personally feel I was inadequate in comforting them and wish I could have done more, but I hope that just being there for them to talk to helped them a little.
Remember, being a resident is different because a) they are already doing rotations in the ED/ICU and so may have a little more comfort in those areas than someone who’s been out of residency for a few years, and b) if I was pulled to the ICU to work in the level as a resident (supervised by a qualified fellow/attending), I would be much less nervous than being pulled to work on the attending level where there is less oversight. Just my $0.02.
(I’m a peds hosptialist and I also am afraid to be pulled into an ICU setting).
Fair point though this was an audience of interns only so no ICU experience yet other than neonatal (picu is a 2nd year rotation).
And very good point about the supervision. They know it wouldn’t be them alone!
this and also I think there is something to ‘the more you know, the more you realize what you don’t know’ – they’ve not only rotated in those areas more recently but they haven’t been working as long as you so maybe don’t realize what they don’t know! But if I were them I’d definitely be fearing working in the ICU. Maybe they have that invincible feeling I had in my 20s still who knows.
For the record, I am an anesthesiologist, and am only a year and a half out from my last critical care rotation, and I would definitely NOT feel comfortable as an attending in a critical care role. I probably do moreso than an endocrinologist who is 10 years out would, but many of the nuances of critical care are really only obtained after doing a fellowship in it. This is most decidedly the case for Emergency Medicine people as well, for whom an even longer critical care fellowship is required to practice than for us. OTOH, could do the resident job without problems.
Sorry, this was meant as a reply to AP below.
I read your blog regularly, but usually don’t comment!
I felt compelled to address the imposter syndrome issue; you are definitely not alone and I think most attendings and residents feel this way right now even if they don’t voice it!
I’m an endocrinology resident, IM trained with recent ICU experience. I have many good friends who are residents in other IM specialties (general internal medicine, etc.) who are truly on the covid-19 frontlines at the moment. A major theme in our conversations lately is fear. Fear of the covid-19 workload and overwhelm, fear of not knowing enough or being able to do techniques well enough, fear of catching covid-19 and spreading it to our loved ones. I think there is really only a very small number of physicians who feel truly comfortable with critical care (like ER, anesthesia, and ICU) and I think the rest of us, even if we did do the training and the procedures, feel very much out of our element in critical care. I try to remind myself that really, few physicians have any training at all for certain ICU techniques and are years away from any acute care medicine, so we are better prepared than most!
I would be afraid to work in the ICU too. But then again I could not be in the health profession either. I am thankful people like you can.
From a non-doctor, I would not qualify your fears as imposter syndrome! Imposter syndrome is when you really are something, but still feel like you are pretending or acting a part. You really are not a critical care doctor. Your fears are totally rational. Any doctor outside that specialty is, by definition, going to be providing care from a less experienced, less knowledgeable place than a practicing critical care doctor. But if that ends up being the situation, that is the reality and you have no ability to control it. Even if you offer less experienced care than a critical care doctor would, the patient is still better off than receiving no care at all due to a shortage of doctors. Totally guessing at your feelings, I would say the fears come from a rational, and good place that you want the best care for all patients you treat and you may be put in the abnormal situation where you can’t do that. But that doesn’t mean you won’t be doing the best you can and offering important service and care to patients.
I think imposter syndrome is widespread. I’m an attorney that’s worked in the same field, child protection and juvenile defense, for 25 years. I’ve done maybe 30 jury trials, and every single time, I feel like I don’t know the law, don’t know the rules of evidence, and I’m just winging it. I think it could be a personality thing, because some people, who really don’t seem competent, are inexplicably confident.
« Not that I truly am qualified to be an ICU physician, but in reality I’m probably the same degree of unqualified as all of my pediatric sub-specialist peers »; in Canada, they asked veterinarian to be ready to be called as backups with some tasks, like handle ventilators… They probably don’t feel 100% qualified, but it is a crisis, they have some skills that are needed.
I’m a medical student and I know imposter syndrome is definitely rampant among my peers (myself included… even though I’m not on the front lines yet, I have been getting SO many questions from friends and family and feel like I know nothing). I also know I probably would not tell my dean or preceptors about feeling that way for fear of judgment, so I’m sure it had to do with the hierarchy more so than them not feeling the imposter syndrome.